
About Mental Health in Guelph
The State of Mental Health in Canada
5.4%
experiences major depression
4.6%
lives with an anxiety disorder
1%
affected by bipolar disorder
1M +
affected by an eating disorder
1%
affected by schizophrenia
6%
face substance use disorders
4,012
died by suicide in 2019
Source: Canadian Mental Health Association (CMHA). Fast Facts about Mental Health and Mental Illness. Link: https://cmha.ca/brochure/fast-facts-about-mental-illness/
Understanding Canada's Student Mental Health Crisis
In a 2021 survey of Canadian post-secondary students, over 40% reported a diagnosed mental illness at some point in their lives.
Within the 12-month period preceding the survey, approximately 30% of students accessed mental health services from their institution or an external provider, highlighting the substantial demand for support.
Anxiety and depression are the most prevalent concerns. Over 50% of students reported experiencing overwhelming anxiety, and a significant portion experienced symptoms of depression that were difficult to manage.
Academic performance is a major stressor. Pressures related to grades, workload, and future career prospects are frequently cited as negatively impacting mental well-being.
Despite the high prevalence, barriers to access remain, including long waitlists for on-campus services, stigma, and financial constraints.


How Mental Health Impacts Canadian Families
Widespread Prevalence: Given that 1 in 5 Canadians experiences a mental illness in any given year, a vast number of families are directly affected. This means most Canadians will have a family member, either immediate or extended, who lives with a mental health condition.
Intergenerational Impact: Parental mental health is a key determinant of children's well-being. The Children’s Mental Health Ontario report states that over 40% of parents say their own mental health challenges have impacted their ability to parent their children.
Systemic Barriers: Families often face significant challenges navigating the healthcare system together, including long wait times for treatment, fragmented services, and financial strain due to therapy costs and lost time at work.
Stigma: Despite progress, stigma remains a barrier. Families can experience social isolation or feel unable to discuss their struggles openly, which can prevent them from seeking help.


The State of Mental Health in the Canadian Workplace
Prevalence is High: In any given week, 500,000 Canadians are unable to work due to mental health issues. This makes mental illness one of the most common causes of workplace disability and absenteeism.
The Burnout Factor: A significant portion of workplace strain is attributed to burnout. Studies have found that over 30% of working professionals report experiencing high levels of mental distress, fatigue, and emotional exhaustion related to their jobs.
The Financial Impact: The economic burden is substantial. Mental health problems and illnesses account for approximately $50 billion annually in costs to the Canadian economy due to lost productivity, healthcare expenditures, and absenteeism and presenteeism (being at work but not fully functioning).
Psychological Safety is Key: Workplaces that promote psychological safety and have clear mental health support systems see significant benefits, including reduced turnover, lower disability costs, and improved overall productivity.


Why Accessible Mental Health Care is Essential?
Accessible mental health care is a cornerstone of a healthy society and a robust economy, not merely a peripheral service. When timely and affordable treatment is available, it enables early intervention, which leads to significantly better recovery rates and prevents conditions from escalating into crises. This proactive approach is far more effective and less costly than dealing with acute emergencies later. Without access, individuals are more likely to require expensive emergency room visits and hospitalizations, placing a severe and preventable strain on the broader healthcare system.

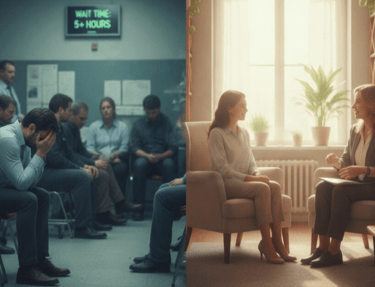
The economic argument is equally compelling. Mental illness costs the Canadian economy over $50 billion annually in lost productivity and healthcare expenditures. Accessible care is a powerful tool to mitigate these losses by helping people remain at work and function effectively. Furthermore, barriers like cost, waitlists, and stigma create profound health inequities, disproportionately impacting vulnerable populations. Investing in accessible care is therefore an investment in overall well-being, system efficiency, and economic productivity, ultimately creating a foundation for a healthier, more resilient society.

Start your path to wellness by booking a free 15-minute consultation with our experienced Counsellors Guelph.
Support
Compassionate counselling and psychotherapy in Guelph.
Care
Growth
34 Harvard Road, unit 2, Guelph, Ontario, N1G 4V8
+1 (437) 826-5358
© 2025. All rights reserved.